‘What Is’ Series: Heart Rate Variability (HRV)
In the high-pressure world of healthcare, where stress, critical decisions, and demanding schedules dominate daily life, having tools to monitor and enhance your well-being isn’t just helpful—it’s essential. Heart rate variability (HRV) is one such game-changing tool. Acting as a barometer of how your body manages stress and recovery, HRV provides a unique lens into your resilience. As a key metric in the Arena Strive experience, it equips you with the insights needed to balance the demands of your profession with personal well-being. Let’s dive into what HRV is, how it’s assessed, and how it can transform the way you approach recovery and performance.
What is HRV and How is it Measured?
HRV is the measurement of the variation in time between consecutive heartbeats, known as R–R intervals (1). Unlike a steady metronome, your heart doesn’t beat in perfect rhythm, and that’s a good thing. These variations reflect the intricate dance between your autonomic nervous system’s two branches:
- Sympathetic Nervous System (SNS): The “fight or flight” responder.
- Parasympathetic Nervous System (PSNS): The “rest and digest” balancer.
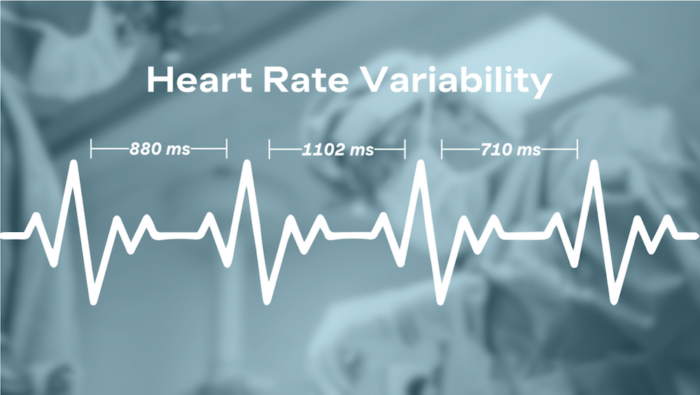
In the past, HRV was most commonly measured using devices like electrocardiograms (ECGs). But in recent years, wearable technologies such as WHOOP, Oura, and Apple Watch have made this data a lot more accessible (2, 3). The two primary methods for calculating HRV are RMSSD (Root Mean Square of Successive Differences) and SDNN (Standard Deviation of Normal-to-Normal Intervals). To establish a consistent baseline, HRV is often captured by these sensors at night, when the body is at rest and external influences like movement and stress are minimized, allowing for a more accurate assessment of autonomic balance and recovery.
The Science Behind HRV
HRV is a direct reflection of your autonomic nervous system’s function, offering insights into your body’s capacity to adapt to physical, mental, and emotional stressors (1). Higher HRV generally indicates better resilience and recovery because it shows that your parasympathetic (rest-and-digest) and sympathetic (fight-or-flight) systems are functioning in balance, allowing your body to respond to stressors efficiently and recover quickly.
Think of it as your body’s “readiness score.” It reflects a state of readiness where stress is well-managed, and recovery is optimized. Conversely, when HRV is low, it suggests that your body may be under strain, signaling the need for rest, recovery, or adjustments in habits to restore balance.
What Impacts HRV?
HRV is influenced by a variety of factors, making it a highly individualized and dynamic measure of health and stress resilience. Here’s a breakdown of some of the key factors impacting HRV:
Positive Influences:
- Regular Physical Activity. Consistent exercise can improve HRV over time, signaling better cardiovascular fitness (4). However, overtraining can lead to a noticeable decline in HRV, making it a critical tool for athletes to monitor recovery and know when they are overdoing it (5).
- Hydration. Staying well-hydrated supports optimal physiological function and can positively affect HRV (6).
Negative Influences:
- Poor Sleep. Insufficient sleep duration or quality directly reduces HRV (7).
- Alcohol Consumption. Alcohol significantly lowers HRV. Wearable devices like Whoop have extensive data illustrating this correlation (8, 9).
- Stress. Both acute and chronic stress negatively impact HRV, as the autonomic nervous system struggles to maintain balance (10).
Other Influences:
- Age. HRV tends to decline with age, although maintaining a healthy lifestyle can slow this process (11).
- Resting Heart Rate (RHR). A higher Resting Heart Rate (RHR) often correlates with lower HRV. Given that HRV measures the variation in time (milliseconds) between consecutive heartbeats. When your RHR is higher, your heart is beating faster, which means there is less time between each heartbeat.
- Sex Differences. Men tend to have slightly higher HRV than women. This is still a ripe research field. One contributing factor is that women generally have higher RHRs due to a smaller heart-to-body ratio, reducing the potential for variation between heartbeats (12, 13).
- Conditions. Given it is a measure of your nervous system and cardiovascular health diseases such as Heart disease or autonomic conditions can impact the metric (1).
Each person’s HRV is shaped by their unique combination of genetics, lifestyle, and environmental factors, making it a personalized indicator of overall health and stress resilience.
How HRV is Used in Performance Industries and Its Potential in Healthcare
Performance industries, such as athletics and the military, have long embraced HRV as a critical tool for optimizing resilience, recovery, and readiness. Elite athletes monitor HRV to fine-tune their training regimens, using it as a guide to balance pushing their limits with adequate recovery (14, 15). Military personnel leverage HRV to assess physiological readiness and ensure they can perform effectively under extreme stress (16). These industries don’t just track HRV—they actively teach individuals to interpret and act on the data, helping them recognize when their bodies are primed for peak performance or in need of recovery.
This same approach can be applied to healthcare, where professionals face similar high-pressure demands. By incorporating HRV tracking, healthcare workers can gain insights into their own resilience and readiness, learning to manage the physical, emotional, and mental stressors that come with their roles. HRV provides an opportunity to:
- Monitor the impact of habits like sleep, nutrition, and mindfulness on overall well-being.
- Recognize when to prioritize rest or recovery.
- Understand how cumulative stress affects performance and implement proactive strategies to manage it.
Meet MJ Wilson, the Director of Clinician Experience at Arena Labs. MJ’s journey bridges the worlds of elite sport and medicine. In October 2023, she competed in the Pan American Games, earning a silver medal in the lightweight double sculls (LW2x). This spring, she will resume medical school, bringing a unique perspective shaped by her experiences as both an elite athlete and a future clinician.
MJ has countless stories of how she integrated HRV into her daily routine and how it played a transformative role. In her role at Arena Labs, MJ leverages her dual background to help clinicians understand the power of HRV in building resilience and supporting recovery in high-pressure environments. Reflecting on her journey of understanding how HRV can used in sport and medicine, she notes:
“I first got my Whoop in 2019 while balancing the demands of a post-baccalaureate pre-med program and full-time rowing in Philadelphia, without the structured support of D1 athletics. Back then, I struggled to prioritize recovery and often pushed myself to the limit – it showed up in sickness, irritability, frustration, and trouble sleeping. My Whoop served as a habit cue to prioritize recovery in the midst of transitioning arenas.
In utilizing Strive, I learned foundational tools–simple practices like breath work and light exposure, and light restriction that aligned with my physiology, to help align my circadian rhythm and activate my parasympathetic nervous system to maximize recovery. I learned how to read and act on my recovery data. I dove into learning more, practicing, and finding what worked best for me; I felt better and saw it in my data. A big unlock was the intentional use of breath work throughout the day, especially after practices, stressful situations, and before going to bed at night.
In rowing, there are two parts to the stroke: the drive and the recovery. Much of your time racing is spent on the recovery, if you can minimize resistance to the boat on the recovery, you can make significant gains in speed because you’re operating more efficiently and leveraging power well. Similarly, our bodies need stressors to create a change, but it is during the recovery that we actually adapt to and become stronger from the stressors. Taking away barriers to recovering well is important!
HRV can be used to look at day-over-day recovery to ensure we don’t take on too much without adapting to it properly. I saw that utilizing breath-work tools and monitoring my recovery made a difference in my physical performance and emotional resilience–ultimately enabling me to be more present in moments that matter – be it the middle of a race, a patient conversation, or limited time with someone I love.”
Your HRV Journey Starts Here
Understanding and leveraging HRV isn’t just about tracking numbers—it’s about unlocking your potential to live and work at your best. With tools like Arena Strive and the support of experienced coaches, you can gain deeper insights into your body’s resilience and learn how to use HRV to enhance your performance and well-being.
To discover more about Arena Strive, or explore bringing it to your hospital, contact us at hello@arenalabs.global.
References:
- Shaffer F, Ginsberg JP. An Overview of Heart Rate Variability Metrics and Norms. Front Public Health. 2017 Sep 28;5:258. doi: 10.3389/fpubh.2017.00258. PMID: 29034226; PMCID: PMC5624990.
- https://www.whoop.com/us/en/thelocker/heart-rate-variability-hrv/
- https://support.ouraring.com/hc/en-us/articles/360025441974-Heart-Rate-Variability#:~:text=illness%2C%20and%20overtraining.-,How%20Oura%20Measures%20HRV,samples%20taken%20while%20you%20sleep.
- Routledge FS, Campbell TS, McFetridge-Durdle JA, Bacon SL. Improvements in heart rate variability with exercise therapy. Can J Cardiol. 2010 Jun-Jul;26(6):303-12. doi: 10.1016/s0828-282x(10)70395-0. PMID: 20548976; PMCID: PMC2903986.
- https://www.trainingpeaks.com/blog/how-monitoring-your-heart-rate-variability-helps-you-avoid-overtraining/
- Young HA, Cousins A, Johnston S, Fletcher JM, Benton D. Autonomic adaptations mediate the effect of hydration on brain functioning and mood: Evidence from two randomized controlled trials. Sci Rep. 2019 Nov 11;9(1):16412. doi: 10.1038/s41598-019-52775-5. PMID: 31712590; PMCID: PMC6848126.
- Bourdillon N, Jeanneret F, Nilchian M, Albertoni P, Ha P, Millet GP. Sleep Deprivation Deteriorates Heart Rate Variability and Photoplethysmography. Front Neurosci. 2021 Apr 8;15:642548. doi: 10.3389/fnins.2021.642548. PMID: 33897355; PMCID: PMC8060636.
- Ralevski E, Petrakis I, Altemus M. Heart rate variability in alcohol use: A review. Pharmacol Biochem Behav. 2019 Jan;176:83-92. doi: 10.1016/j.pbb.2018.12.003. Epub 2018 Dec 6. PMID: 30529588.
- https://www.whoop.com/us/en/thelocker/how-alcohol-negatively-impacts-your-biometic-data/?srsltid=AfmBOop8Rgagoy6erDAa4DbCLD2teCiF2XbQhOEOAJBEvji_PzbZQ_TC
- Kim HG, Cheon EJ, Bai DS, Lee YH, Koo BH. Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature. Psychiatry Investig. 2018 Mar;15(3):235-245. doi: 10.30773/pi.2017.08.17. Epub 2018 Feb 28. PMID: 29486547; PMCID: PMC5900369.
- https://www.whoop.com/us/en/thelocker/what-is-a-good-hrv/
- Umetani K, Singer DH, McCraty R, Atkinson M. Twenty-four hour time domain heart rate variability and heart rate: relations to age and gender over nine decades. J Am Coll Cardiol. 1998 Mar 1;31(3):593-601. doi: 10.1016/s0735-1097(97)00554-8. PMID: 9502641.
- https://www.whoop.com/us/en/thelocker/normal-hrv-range-age-gender/
- https://www.whoop.com/us/en/thelocker/patrick-mahomes-the-data-behind-a-season-with-whoop/?srsltid=AfmBOorKOMKpTZIxfLTvbRaL0Uy20bWqD2aiMJUzNDrhasQ9CG_toR75
- https://www.nytimes.com/athletic/5564250/2024/06/14/england-oura-ring-southgate/
- https://www.army.mil/article/278986/monitoring_army_aviators_in_flight_heart_rate_variability_during_extreme_maneuvering