Residency is an intensive, years-long training period where newly minted doctors transition from medical school to full-time clinical practice, often working long hours under high stress. By the first year of residency, many young doctors already experience moderate depersonalization, emotional exhaustion, and burnout. These aren’t just abstract ideas—they manifest in physiological changes that impact cognitive function, decision-making, and long-term health.
For the first time, consumer-grade wearable sensors allow us to analyze biometric trends at a population level. This technology provides an opportunity to better support medical teams by offering insights into Heart Rate Variability (HRV), sleep duration, and sleep debt. By understanding the reality of your team’s physiology and trends, you have the agency to set the tone as a leader—guiding how they care for themselves, support one another, and how you show up for them.
Why Does This Matter? HRV measures the variation in time between heartbeats and provides a snapshot of the nervous system’s balance—essentially, the body’s ability to manage stress and recover. While HRV is highly individualized, a simple rule of thumb applies: higher is better, lower signals stress. For example, by tracking group trends in a group of residents, we can begin to ask critical questions: What led to an increase in HRV? What factors contributed to a decrease? Similarly, sleep duration and sleep debt play a crucial role in overall recovery. Sleep is essential for cognitive function, decision-making, and physical restoration. When sleep debt accumulates—meaning residents consistently get less sleep than their bodies require—cognitive performance, reaction time, and emotional regulation suffer.
Learn more about HRV here.
In this blog, we’ll explore:
- Sleep debt patterns in residency and their implications
- What HRV and sleep duration reveal about recovery
- How performance coaching can optimize well-being
- A case study from aviation: how decision-makers acted on similar data
The Sleep Deficit: A Daily Battle
Our data from the Arena Strive platform shows that residents average 6 hours and 38 minutes of sleep per night—falling short of the CDC-recommended 7+ hours (1). On weekends, they manage to sleep 40 minutes longer, but this is nowhere near enough to offset the cumulative deficit accrued during the workweek.
The data paints a clear picture: a steady accumulation of sleep debt throughout the week, followed by only minor recovery on days off. By the end of the week, residents accumulate over two hours of sleep debt—extrapolated over time, this adds up to more than 100 hours of missing sleep per year.
Total 7-day Sleep Debt: 2 hours 26 minutes
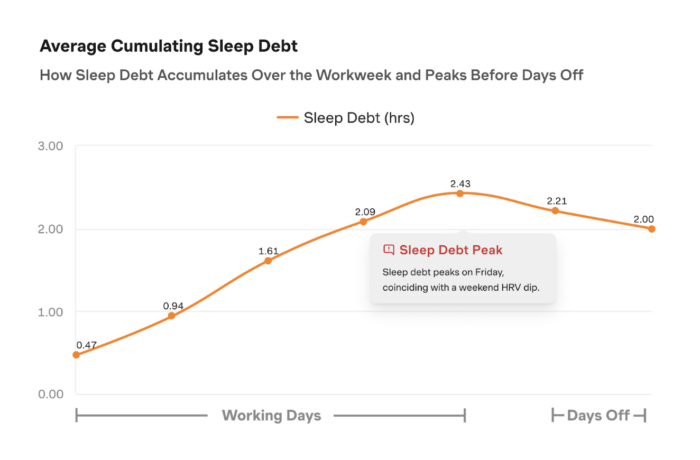
A common belief among high-achieving individuals is that they can function well on limited sleep. However, as neuroscientist Matthew Walker puts it, “The percentage of the population that can survive on six hours of sleep or less without measurable impairment, rounded to a whole number, is zero. (2–4)” Even small amounts of lost sleep have consequences: a 2021 WHOOP study found that just 45 minutes of sleep debt results in a 5–10% decline in executive function and cognitive control—skills essential for high-stakes decision-making (5).
To be clear, this isn’t a critique of residents. Their schedules are dictated by external demands. Similar sleep challenges exist in other high-performance fields, including elite military units, professional sports, and aviation. The difference? In most of these other industries, leadership actively addresses fatigue management, and individuals are trained in understanding how to optimize their recovery – even without 8 hours of sleep. As our founder Brian Ferguson notes, “Healthcare is the last industry where it’s a badge of honor to not get sleep.”
For individuals, simply understanding their physiological limits can improve performance. For leaders, recognizing team-wide trends offers a chance to set a culture that balances rigor with care.
Using HRV to Identify Opportunities for Improvement
Beyond sleep debt, HRV and resting heart rate trends provide valuable insight into the physiological toll of residency. Interestingly, HRV tends to drop on weekends, even when sleep duration increases. Resting heart rate also tends to spike during time off.
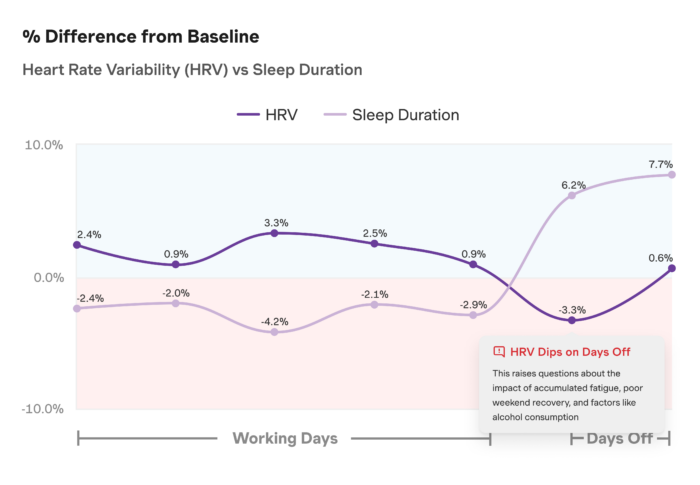
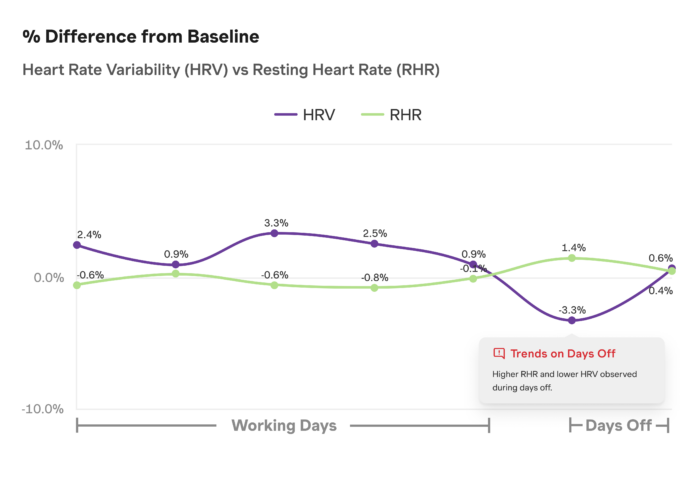
What does this mean? While additional sleep is helpful, recovery isn’t just about quantity—it’s about quality. Several factors could contribute to this trend, including accumulated stress, disrupted circadian rhythms, or lifestyle habits on days off. A similar phenomenon was observed in a previous case study on active recovery (read more here).
While these trends may seem discouraging, the reality is that awareness creates opportunity. One of our performance coaches reflected:
“It’s interesting to see the cumulative impact of sleep debt on HRV. While residents gain extra sleep on weekends, they’re still operating at a disadvantage. The body doesn’t fully adapt to chronic sleep deprivation, and shifts in sleep schedules likely contribute to their fatigue. Optimizing recovery isn’t about achieving perfection—it’s about maximizing what’s within control. That means focusing on sleep efficiency, creating an optimal sleep environment, and adopting small recovery strategies within the constraints of residency.”
Simply put, if time is limited, efficiency matters. The time spent in bed should be as restorative as possible. Sleep quality improvements—such as optimizing the sleep environment or adjusting pre-bedtime habits—can make a significant difference in overall recovery.
What Leaders from Other High-Stakes Professions Get Right
While residency schedules are demanding, this challenge isn’t unique to medicine. Other high-stakes professions have acknowledged the risks of sleep deprivation and cognitive impairment—and have taken action.
Consider aviation: The FAA regulates crew rest, ensuring pilots receive mandated recovery periods between shifts. These rules are based on fatigue science and balance operational demands with human performance needs. Pilots must have at least 24 consecutive hours off every seven days (6)—a stark contrast to the unpredictable, extended shifts common in medicine.
Knowing how fatigue impacts performance allows leaders to make informed decisions about team structure, workload, and recovery opportunities. It’s not just about policies—it’s about culture. How leaders show up for their teams determines how teams show up for their work. This data set is missing in healthcare organizations.
Residency is not just a test of endurance; it’s a critical training ground for the future of healthcare. The habits, resilience, and self-awareness that young clinicians develop now will shape how they show up for patients for years to come. Leaders who prioritize performance optimization during this stage aren’t just helping their teams today—they’re shaping the future of medicine.
If you’re interested in exploring what’s possible for your hospital, reach out to us at hello@arenalabs.co.
Want to learn more about Predictive Performance™? Contact joshua@arenalabs.co.
Sources: